Deepening Your Understanding of the NHS Funding Framework
The NHS funding framework is an essential cornerstone of financial management within the UK healthcare system, creating a robust structure that dictates the allocation of resources across a wide array of services nationwide. It is imperative for stakeholders, including healthcare administrators, policymakers, and financial managers, to grasp the intricacies of this framework. By doing so, they can adeptly navigate the complex terrain of healthcare financial growth and sustainability, ensuring effective resource distribution and service delivery across the board.
Diving into the NHS Budget Distribution Mechanism

The budget distribution process within the NHS is a carefully crafted mechanism designed to guarantee that financial resources are allocated to areas of utmost need. NHS England utilises a sophisticated formula for resource distribution, which takes into consideration several factors, including population size, demographic diversity, and specific health requirements across various regions. This allocation process is significantly guided by the principle of equitable access to healthcare services, aiming to reduce disparities among different geographical locations. Consequently, it ensures that all communities receive adequate and fair treatment, thus promoting health equity across the nation.
Each fiscal year, the budget undergoes meticulous scrutiny and approval by the government, reflecting the current policies and healthcare priorities that are in place. This allocation covers essential services, such as mental health care, community health initiatives, and preventive health measures, fostering a holistic approach to healthcare delivery. By comprehending these dynamics, healthcare administrators and policymakers can align their operational strategies more effectively with the available financial resources, thereby facilitating effective management of healthcare financial growth and enhancing overall service provision.
Moreover, regional disparities can drastically affect the availability and quality of healthcare services. For instance, rural areas frequently experience challenges in securing sufficient funding compared to urban regions. This issue necessitates innovative strategies from healthcare providers to secure additional funding and maintain service quality, regardless of geographical constraints. By addressing these disparities, the NHS can work towards a more equitable healthcare system that meets the needs of all populations, thereby improving overall health outcomes.
Examining the Impact of Government Policies on NHS Funding
Government policies serve as crucial levers that shape NHS funding and influence the financial strategies employed within the healthcare sector. Decisions concerning healthcare expenditure reflect broader political agendas and prevailing economic conditions. For example, the government may launch initiatives aimed at reducing patient waiting times or enhancing mental health services, directly impacting the allocation of funds across various sectors within the NHS.
Policies such as the Five Year Forward View illustrate a commitment to integrated healthcare and community-based services, advocating for a shift away from traditional hospital-centric care models. These transformative changes compel healthcare providers to adapt their financial strategies, ensuring alignment with policy directives that promote sustainability and operational efficiency throughout the system.
Additionally, the introduction of policies that incentivise innovation, exemplified by initiatives like the Health Innovation Network, can significantly boost financial growth by encouraging the adoption of novel approaches to care delivery and operational efficiency within the NHS framework. This proactive approach not only fosters a culture of innovation but also enhances the overall quality of healthcare services delivered to patients.
Implementing Strategic Long-Term Financial Planning for the NHS
Strategic long-term financial planning is vital for the NHS as it navigates an increasingly complex healthcare landscape. Effective planning involves forecasting future healthcare demands while considering demographic changes and anticipating economic fluctuations. By preparing for these evolving variables, healthcare organisations can develop robust financial strategies that support sustainable growth and adaptability in their service delivery models, ensuring they remain responsive to community needs.
Forming strategic partnerships and collaborations plays a crucial role in long-term planning, enabling organisations to pool resources and share the risks associated with significant financial investments. For instance, working closely with local authorities and community organisations can facilitate the development of integrated services that comprehensively address patient needs while ensuring financial viability and sustainability. This collaborative approach fosters a more cohesive healthcare delivery system that can effectively respond to diverse patient populations.
Furthermore, incorporating risk management into long-term financial planning significantly enhances an organisation’s capacity to respond to unforeseen challenges. This proactive strategy includes preparing for potential funding cuts or shifts in governmental policy, thereby ensuring that healthcare providers maintain resilience and adaptability in an increasingly turbulent financial environment. By prioritising risk management, organisations can safeguard their financial health while continuing to provide essential services to their communities.
Exploring Diverse Sources of NHS Funding
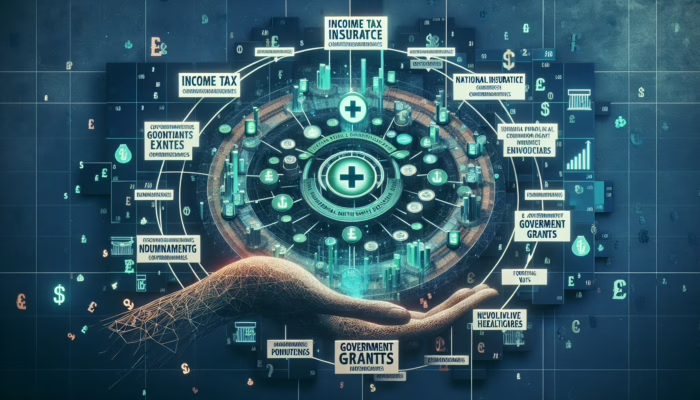
The NHS primarily relies on taxation for funding, with the public contributing through income tax, national insurance contributions, and VAT. Understanding the diversity of these funding sources is crucial for comprehending the financial landscape of the NHS. Each funding source carries implications for financial stability and growth, as economic fluctuations can directly impact tax revenues and, consequently, the funds available for healthcare services.
In addition to traditional taxation, the NHS benefits from government grants aimed at financing specific initiatives, such as technological advancements or public health campaigns. These grants serve as critical financial supports, enabling the implementation of innovative programmes that enhance service delivery and improve patient care across the healthcare system. By accessing these funds, healthcare organisations can invest in initiatives that directly benefit the community and enhance overall health outcomes.
Moreover, partnerships with the private sector can introduce alternative revenue streams. Engaging in joint ventures or public-private partnerships (PPPs) allows the NHS to explore funding opportunities that might not be accessible through conventional channels. This strategic collaboration strengthens the overall financial structure of healthcare providers and supports long-term sustainability, ensuring that they can continue to deliver high-quality care to patients.
Maximising the Benefits of Private Sector Collaborations
The growing trend towards public-private partnerships (PPPs) signifies a transformative shift in how the NHS approaches financial growth and service delivery. By leveraging the strengths and resources of private organisations, the NHS can optimise its resources, enhance the quality of services provided, and ultimately achieve better patient outcomes. This collaborative model not only aids financial sustainability but also fosters innovation in healthcare delivery.
Understanding Public-Private Partnerships (PPPs) in Healthcare
Public-private partnerships represent a strategic collaboration where the public sector works closely with private organisations to deliver healthcare services more efficiently and effectively. This model allows for shared investment responsibilities, reducing the financial burden on the NHS while simultaneously enhancing the scope and quality of service provision. By pooling resources and expertise, these partnerships can lead to significant improvements in patient care and operational efficiency.
One of the most notable advantages of PPPs is the potential for improved infrastructure development. For instance, private companies can take the lead in constructing and managing healthcare facilities, thereby freeing NHS resources to focus on critical services. This cooperative approach can result in faster project completion times and superior quality in facility management, ultimately enhancing patient experiences across the board and improving access to necessary care.
Moreover, PPPs can facilitate the introduction of innovative practices and advanced technologies that the NHS may find challenging to implement independently due to budget constraints. By harnessing the expertise and efficiencies inherent in the private sector, the NHS can remain at the forefront of effective healthcare delivery and innovation, ensuring that patients receive the best possible care tailored to their needs.
The Role of Private Investment in Advancing Healthcare Development

Private investment has increasingly become a vital component of the financial growth strategies within the NHS. Such investments can support infrastructural developments and technological advancements that significantly enhance patient care and service delivery across the board. By fostering these investments, the NHS can improve its overall capabilities and service offerings, leading to better health outcomes for patients.
Investment from venture capital and private equity firms often targets groundbreaking healthcare solutions, driving advancements in medical technologies and innovative service delivery models. For instance, investments in telemedicine can dramatically expand access to care, particularly in underserved regions, while also generating additional revenue streams for healthcare providers. This not only enhances patient access but also contributes positively to the financial sustainability of healthcare operations.
However, attracting private investment necessitates a transparent and well-articulated value proposition. By demonstrating potential returns on investment and showcasing successful case studies, healthcare organisations can encourage private entities to engage with the NHS, thereby positively contributing to effective management of healthcare financial growth. This collaborative approach ensures that both parties benefit from the investment, ultimately enhancing the quality of healthcare services available to patients.
Navigating the Regulatory Framework for Successful Partnerships
The regulatory environment governing private sector partnerships in the UK healthcare system is crucial for ensuring that collaborations are conducted ethically and sustainably. Understanding this regulatory framework is essential for stakeholders seeking to engage in public-private partnerships (PPPs) to ensure compliance and maintain public trust.
Regulations establish standards for quality, accountability, and transparency, which are vital for maintaining public trust in the NHS. The Care Quality Commission (CQC) plays a pivotal role in assessing the performance of both public and private healthcare providers, setting benchmarks that must be met to ensure patient safety and quality of care. This regulatory oversight ensures that partnerships contribute positively to the healthcare system while safeguarding patient interests.
Additionally, robust contractual agreements must clearly outline the responsibilities and expectations of each party involved in a PPP. This legal framework fosters a cooperative environment where innovation can flourish while adhering to the overarching objectives of public health and patient welfare. By ensuring clarity and accountability, these agreements help mitigate risks and facilitate successful collaboration between public and private entities.
Exploring Successful Case Studies of Public-Private Partnerships
Examining real-world examples of effective private sector partnerships underscores the potential benefits that can arise from collaborative efforts within the NHS. One notable instance involves the collaboration between the NHS and private healthcare providers in addressing elective surgeries. This partnership enabled private facilities to perform elective procedures on behalf of the NHS, significantly reducing patient waiting times and enhancing service delivery.
This arrangement not only benefited patients by providing quicker access to necessary procedures but also allowed the NHS to reallocate its resources towards more urgent care needs. This practical application of effective management of healthcare financial growth demonstrates how public-private partnerships can lead to improved efficiency and better patient outcomes while optimising resource utilisation.
Another compelling example can be found in the collaboration between the NHS and technology firms in implementing electronic health record systems. By partnering with private technology companies, the NHS has streamlined its data management processes, enhancing patient care and operational efficiency. These partnerships exemplify how leveraging private sector expertise can lead to tangible improvements in both service delivery and financial sustainability within the healthcare framework.
Implementing Cost-Effective Healthcare Solutions for Enhanced Efficiency
The drive towards cost-effectiveness in healthcare transcends the mere act of cutting expenses; it revolves around maximising value and improving health outcomes for patients. Implementing cost-effective solutions necessitates a multifaceted approach that integrates technology, preventive care, and efficient administrative processes to achieve optimal results in healthcare service delivery.
Harnessing Technology to Revolutionise Healthcare Delivery
The integration of advanced technology in healthcare delivery is paramount for achieving significant cost efficiencies. Innovations such as electronic health records (EHRs), telehealth services, and AI-driven diagnostics are revolutionising how care is provided, leading to substantial cost savings and enhanced patient experiences. By adopting these technologies, healthcare providers can improve their overall operational efficiency and service delivery.
For example, EHRs streamline documentation processes and reduce time spent on administrative tasks, allowing healthcare professionals to dedicate more time to direct patient care. This efficiency can translate into lower operational costs and heightened patient satisfaction, making technology a vital component of effective management of healthcare financial growth. By leveraging technology, the NHS can enhance its service capabilities and improve patient outcomes significantly.
Telehealth services have emerged as a transformative solution, especially in remote areas where access to care may be limited. By facilitating virtual consultations, healthcare providers can reduce overhead costs while simultaneously expanding their reach and service availability. This model not only enhances patient access to care but also optimises resource utilisation, ultimately contributing to the financial health of the NHS and ensuring that patients receive timely and effective care.
Investing in Preventive Care Initiatives for Long-Term Savings
Investing in preventive care initiatives stands out as one of the most effective strategies for mitigating long-term healthcare costs. By prioritising prevention over mere treatment, the NHS can alleviate the financial burdens associated with chronic diseases and enhance overall public health outcomes. This shift towards preventive care not only benefits individual patients but also supports the healthcare system’s sustainability in the long run.
Preventive programmes, including vaccinations and routine health screenings, not only bolster public health but also significantly reduce hospital admissions and emergency care costs. The recent emphasis on promoting healthy lifestyles through public health campaigns has demonstrated how a proactive approach can yield substantial financial benefits for the healthcare system. By focusing on prevention, the NHS can create a healthier population and reduce the overall demand for costly medical interventions.
Moreover, leveraging data-driven insights can help healthcare providers identify at-risk populations, allowing them to target interventions more effectively. This strategic emphasis on prevention not only improves individual patient health but also supports the financial sustainability of healthcare services across the board. By investing in preventive care, the NHS can achieve significant long-term savings while improving health outcomes for the entire community.
Streamlining Administrative Processes for Enhanced Efficiency
Administrative inefficiencies can severely drain resources and hinder the financial growth of healthcare organisations. Streamlining these processes is essential for enhancing operational performance and ensuring that funds are directed to frontline services where they are most needed. By optimising administrative functions, healthcare providers can improve their overall efficiency and financial performance.
Implementing best practices, such as centralising administrative functions or adopting automated systems, can lead to significant cost reductions. For instance, integrating billing systems can minimise errors and expedite revenue collection, thus improving overall financial performance within healthcare organisations. By enhancing administrative efficiency, organisations can free up resources to invest in patient care and service enhancements.
Continuous training and development of administrative staff also play a crucial role in optimising processes. By equipping employees with the skills necessary to navigate complex systems effectively, healthcare organisations can enhance their operational efficiency, ultimately benefiting their financial bottom line and overall service delivery. A well-trained administrative workforce contributes to smoother operations, allowing healthcare providers to focus on delivering high-quality care to patients.
Enhancing Revenue through Strategic Service Diversification
Service diversification emerges as a vital strategy for enhancing revenue streams within the NHS. By broadening the range of services offered, healthcare providers can attract new patient demographics and ensure long-term financial stability. This approach not only enhances the organisation’s financial health but also improves patient access to necessary services.
Expanding Access to Outpatient Services for Increased Revenue
Expanding outpatient services is an effective method for increasing revenue while simultaneously enhancing patient care. Outpatient care alleviates pressure on inpatient facilities and offers a more cost-effective alternative for patients requiring services such as diagnostics or minor surgical procedures. By investing in outpatient facilities and services, healthcare organisations can tap into the growing demand for convenient care options, which not only improves patient satisfaction but also generates additional revenue.
This shift towards outpatient care models is increasingly becoming essential in addressing healthcare demands and optimising resource allocation. For instance, developing specialised outpatient clinics focusing on chronic disease management can cater to specific patient populations, ensuring that services are tailored to meet their unique needs. This targeted approach not only enhances service quality but also contributes to the organisation’s financial performance and sustainability in the long run.
By broadening the scope of outpatient services, healthcare providers can increase patient throughput, reduce waiting times, and ultimately enhance the overall patient experience. This strategy not only improves access to care but also optimises resource utilisation, leading to improved financial outcomes for healthcare organisations.
Establishing Specialist Care Units for Revenue Growth and Enhanced Care
The establishment of specialised care units within the NHS can significantly enhance financial growth by attracting referrals and increasing service utilisation. These units can focus on specific areas such as cardiology, orthopaedics, or oncology, providing targeted services that effectively meet the needs of particular patient groups. By creating these specialised units, healthcare organisations can position themselves as leaders in specific fields of care, drawing patients from surrounding areas and thereby enhancing their reputation in the process.
This competitive advantage can lead to increased revenue and improved financial stability, benefitting the overall healthcare system. Additionally, the creation of specialist units can facilitate collaborations with academic institutions, potentially unlocking additional funding for research and innovation, which can further support financial growth and the advancement of healthcare practices.
By focusing on specialised care, healthcare providers can offer higher quality services tailored to the unique needs of patients, thereby improving overall patient outcomes and satisfaction. This targeted approach not only enhances the organisation’s reputation but also contributes to its long-term financial health and sustainability.
Integrating Telehealth Services into Care Delivery for Broader Reach
The introduction of telehealth services presents a unique opportunity for the NHS to diversify its revenue streams while simultaneously improving patient access to care. By offering remote consultations, healthcare providers can cater to patients who may be unable to attend in-person appointments, thereby extending their reach and enhancing service accessibility. This model not only improves patient access but also contributes to the financial sustainability of healthcare operations.
Telehealth enables healthcare organisations to optimise their resources, as virtual consultations typically require fewer overhead costs than traditional face-to-face visits. This efficiency not only enhances patient satisfaction but also contributes positively to the financial health of healthcare providers. By integrating telehealth into service delivery, the NHS can better meet the needs of diverse patient populations, thereby improving overall health outcomes.
Moreover, as digital health technologies continue to evolve, the potential for integrating telehealth with other services grows, creating new pathways for revenue generation and improving overall patient outcomes in the process. This strategic integration allows healthcare providers to enhance their capabilities and ensure that they remain responsive to patient needs.
Implementing Comprehensive Wellness Programmes for Health Promotion
Wellness programmes embody a proactive approach to healthcare that can attract new patient demographics and contribute to financial growth. By concentrating on prevention and health promotion, these programmes can significantly reduce healthcare costs associated with chronic diseases and enhance overall community health. This strategic emphasis on wellness not only benefits individual patients but also supports the sustainability of healthcare services.
Such initiatives can encompass health screenings, lifestyle coaching, and fitness classes, encouraging participants to proactively take charge of their health. As awareness of wellness increases, healthcare providers can leverage these trends to attract patients seeking preventive services, thus enhancing their revenue base and expanding their community footprint. By fostering community engagement, organisations can enhance their reputation and establish long-lasting relationships with the populations they serve.
Moreover, establishing partnerships with local businesses to offer corporate wellness programmes can create additional revenue opportunities, allowing healthcare organisations to reach new audiences and promote healthier communities. This collaborative approach not only supports the financial health of healthcare providers but also contributes positively to the overall well-being of the community, fostering a culture of health and wellness.
Strategically Managing Healthcare Workforce Costs for Financial Sustainability
Strategically managing workforce costs is a critical component of sustaining financial growth within the NHS. Given that the workforce represents one of the largest expenses for healthcare organisations, it is imperative to optimise resources without compromising the quality of care delivered to patients. By effectively managing workforce costs, healthcare providers can ensure that they maintain high standards of care while remaining financially viable.
Optimising Staffing Levels for Enhanced Financial Efficiency
Optimising staffing levels is essential for effectively managing workforce costs while maintaining high standards of patient care. Overstaffing can lead to unnecessary expenses, while understaffing may compromise service delivery and patient outcomes. Therefore, it is crucial for healthcare organisations to strike a balance that ensures adequate staffing during peak periods while avoiding excess costs.
Utilising data analytics to assess patient demand and staff utilisation can significantly inform staffing decisions. By understanding peak times and resource needs, healthcare managers can adjust staffing levels accordingly, ensuring that the appropriate number of staff is available during critical periods. This data-driven approach not only enhances operational efficiency but also ensures that patient care remains a top priority.
Furthermore, adopting flexible staffing models, such as employing part-time or agency staff during peak periods, can enhance operational efficiency without incurring substantial costs. By implementing such strategies, healthcare organisations can maintain financial health while ensuring that patient care standards are upheld, ultimately benefiting both patients and the organisation.
Investing in Staff Training and Development Initiatives for Improved Performance
Investing in training and development initiatives for healthcare staff can profoundly impact workforce efficiency and financial growth. By equipping employees with the latest skills and knowledge, healthcare organisations can significantly enhance their service delivery capabilities and patient care outcomes. This commitment to staff development not only improves operational performance but also fosters employee satisfaction and retention.
Training programmes that emphasise interdisciplinary collaboration can improve communication and teamwork among staff members, leading to better patient outcomes and increased operational efficiency. Moreover, well-trained staff members are more likely to remain engaged and satisfied in their roles, reducing turnover rates and associated recruitment costs. By investing in workforce development, healthcare organisations can build a resilient and capable team.
Additionally, fostering a culture of continuous professional development encourages staff to explore innovative ways to improve processes and patient care. This culture of learning not only enhances the organisation’s overall performance but also contributes positively to the financial health and sustainability of healthcare services.
Implementing Flexible Work Arrangements for Staff Satisfaction and Retention
Implementing flexible work arrangements can serve as a strategic tool for managing workforce costs while simultaneously promoting employee satisfaction. Offering options such as remote work, flexible hours, or job-sharing can significantly enhance work-life balance for healthcare staff members. By prioritising employee well-being, organisations can create a more positive work environment that fosters engagement and productivity.
These flexible arrangements can lead to reduced absenteeism, improved retention rates, and heightened morale among employees. As staff members feel more valued and supported in their roles, they are likely to provide better patient care, ultimately contributing to the financial sustainability of the healthcare organisation. This positive impact on patient care aligns with the overarching goals of the NHS to provide high-quality services to the community.
Furthermore, such flexibility can attract a broader talent pool, including individuals who may have previously felt unable to commit to traditional work schedules. By embracing diverse work arrangements, healthcare organisations can strengthen their workforce and enhance overall organisational effectiveness, ensuring that they are well-equipped to meet the evolving needs of patients.
Securing Additional Funding Sources for Sustainable Financial Growth
In an environment characterised by tightening budgets, securing additional funding sources is vital for enhancing healthcare financial growth. By diversifying funding streams, healthcare organisations can bolster their financial stability and ensure continued service delivery to the communities they serve. This proactive approach to funding is essential for maintaining high-quality care in an increasingly competitive healthcare landscape.
Pursuing Grants and Subsidies for Targeted Healthcare Initiatives
Grants and subsidies represent significant opportunities for healthcare organisations seeking additional funding to support a variety of initiatives. These financial aids can facilitate projects ranging from research and innovation to infrastructure improvements and service enhancements. By actively pursuing these opportunities, healthcare organisations can secure the resources necessary to enhance their service offerings and improve patient care.
Organisations can actively pursue grants from government agencies, charitable foundations, and private organisations. Crafting compelling proposals that highlight the potential impact of proposed projects is essential for successfully attracting funding and support. By demonstrating the value of their initiatives, healthcare organisations can increase their chances of securing the funding they need to thrive.
Moreover, understanding the criteria for various grants and aligning project goals with funder priorities can significantly increase the likelihood of securing support. This proactive approach to funding can enhance financial growth and empower organisations to invest in critical services and initiatives that benefit patient populations. By focusing on projects that align with funder interests, healthcare organisations can build lasting relationships and secure ongoing support for their initiatives.
Harnessing Fundraising and Donations for Community Support and Engagement
Fundraising and donations play a crucial role in supporting healthcare financial growth, particularly for community-based organisations and charitable initiatives. Engaging the local community in fundraising efforts can foster strong relationships and generate vital resources to support healthcare services. By building a sense of community ownership, organisations can enhance their financial capabilities and ensure sustainable service delivery.
Implementing diverse fundraising strategies, from charity events to online crowdfunding campaigns, can significantly enhance financial capabilities. By creating compelling narratives around healthcare needs and success stories, organisations can inspire individuals and businesses to contribute generously to their causes. This community engagement not only provides crucial financial support but also strengthens community ties and promotes awareness of local health issues.
Moreover, establishing a dedicated fundraising team can streamline efforts and ensure that campaigns are effectively managed and promoted. This coordinated approach enhances the organisation’s financial health and capacity to provide essential services to the community. By prioritising fundraising initiatives, healthcare organisations can secure the resources necessary to expand their services and meet the evolving needs of their patients.
Collaborating with Research Institutions for Shared Funding Opportunities
Collaborating with research institutions can unlock additional funding opportunities that drive healthcare financial growth. Joint research initiatives can lead to grants and sponsorships while simultaneously enhancing the organisation’s reputation for innovation and excellence in healthcare delivery. These partnerships not only provide funding but also foster a culture of collaboration and knowledge exchange.
Such collaborations can focus on areas such as clinical trials, health services research, or public health studies, creating synergistic benefits for all parties involved. By leveraging the expertise and resources of research institutions, healthcare organisations can access new funding streams that enhance their service offerings and improve patient care outcomes. This collaborative approach strengthens the organisation’s capabilities and enhances its overall impact on community health.
Moreover, successful collaborations can result in published studies and recognition within the academic community, further promoting the organisation’s commitment to advancing healthcare and improving health outcomes for diverse populations. By engaging in research partnerships, healthcare organisations can position themselves as leaders in the field and attract additional support for their initiatives.
Engaging the Private Sector for Investment Opportunities and Sustainable Growth
Attracting investments from the private sector can significantly bolster healthcare funding and support financial growth initiatives. This strategy requires a clear articulation of value propositions and potential returns on investment for private investors who may be interested in supporting healthcare initiatives. By presenting a compelling case for investment, healthcare organisations can secure the resources necessary to enhance their capabilities and expand their services.
Establishing partnerships with private companies can lead to joint ventures or funding for specific initiatives, such as technological advancements or service expansions. These collaborations can enhance the infrastructure and capabilities of healthcare providers, creating mutual benefits for both parties involved in the partnership. By leveraging private sector expertise, healthcare organisations can improve operational efficiency and service delivery, ultimately benefiting patients.
Additionally, engaging with investors who share a commitment to improving health outcomes can strengthen relationships and foster ongoing financial support. This collaborative approach not only enhances the organisation’s financial stability but also ensures that healthcare providers can continue to deliver high-quality services to their communities. By building strong partnerships, healthcare organisations can secure the resources necessary for sustainable growth and innovation.
Navigating Government Funding Programs for Strategic Support and Development
Understanding the various government funding programmes available is essential for healthcare organisations aiming to secure financial stability and growth in an increasingly competitive environment. These programmes often focus on specific initiatives, such as mental health services or technology upgrades, offering targeted support that can significantly enhance service delivery. By actively engaging with these funding opportunities, healthcare organisations can bolster their financial capabilities and improve patient care.
Healthcare organisations can actively engage with local health authorities to identify funding opportunities that align with their strategic goals and objectives. Crafting proposals that effectively highlight the potential impact of proposed projects can enhance the likelihood of securing government support and collaboration. This proactive approach to funding is crucial for ensuring that organisations can access the resources needed to thrive in a challenging environment.
Moreover, staying informed about changes in government policy and funding priorities allows organisations to adapt their strategies effectively, maximising available resources and enhancing their financial growth prospects in the process. By remaining agile and responsive to funding opportunities, healthcare organisations can ensure their long-term sustainability and resilience.
Monitoring and Evaluating Financial Performance for Sustainable Growth
Monitoring and evaluating financial performance is a fundamental aspect of ensuring sustainable growth within the NHS. By establishing clear metrics and continuously assessing performance, healthcare organisations can identify areas for improvement and optimise their financial strategies for enhanced effectiveness. This systematic approach to financial management is essential for maintaining operational efficiency and ensuring that resources are utilised effectively.
Establishing Key Performance Indicators (KPIs) for Financial Health Monitoring
Establishing key performance indicators (KPIs) is vital for monitoring the financial health of healthcare organisations. KPIs provide valuable insights into various aspects of financial performance, from revenue generation to cost management and operational efficiency. By implementing a robust framework for KPI monitoring, organisations can gain a clearer understanding of their financial standing and identify areas that require attention.
Healthcare providers can utilise KPIs to track progress against financial goals, identifying trends and patterns that inform decision-making and strategic planning. For instance, monitoring patient volume, average length of stay, and revenue per service line can offer insights into operational efficiency and profitability, allowing for informed adjustments as needed. By aligning KPIs with strategic objectives, healthcare organisations can ensure that their financial strategies are optimally focused on achieving desired outcomes.
Regularly reviewing KPIs not only enhances accountability but also empowers organisations to make data-driven decisions that drive financial growth. This proactive approach to financial management ensures that organisations remain agile and responsive to changing circumstances, ultimately contributing to their long-term viability and success.
Conducting Regular Financial Audits for Transparency and Accountability
Conducting regular financial audits is essential for ensuring transparency and accountability within healthcare organisations. Audits provide an independent assessment of financial practices, identifying potential areas for improvement and ensuring compliance with regulatory requirements and standards. This systematic approach to auditing enhances financial management practices and fosters a culture of accountability within the organisation.
By establishing a routine audit process, organisations can gain insights into their financial operations, enhancing financial management practices and fostering a culture of accountability. This proactive approach to auditing ensures that resources are used efficiently and effectively, ultimately contributing to overall financial health and sustainability. By prioritising transparency, healthcare organisations can build trust with stakeholders and enhance their reputation within the community.
Moreover, the findings from audits can inform strategic planning and decision-making, enabling organisations to make informed choices that support their long-term financial growth and operational effectiveness. By leveraging audit insights, healthcare providers can optimise their financial strategies and ensure that they remain responsive to emerging challenges and opportunities.
Adopting Continuous Improvement Strategies for Enhanced Financial Performance
Adopting continuous improvement strategies is fundamental to enhancing financial performance and growth within the NHS. By fostering a culture of innovation and responsiveness, healthcare organisations can adapt to changing circumstances and optimise their operations accordingly. This commitment to continuous improvement is vital for ensuring that organisations remain competitive in an evolving healthcare landscape.
Implementing methodologies such as Lean, Six Sigma, or Total Quality Management can streamline processes, reduce waste, and enhance overall efficiency. By regularly assessing operations and identifying opportunities for improvement, organisations can ensure that they are consistently delivering value to patients while managing costs effectively. This focus on operational excellence contributes to the long-term sustainability of healthcare services.
Furthermore, encouraging staff participation in improvement initiatives can lead to innovative solutions that enhance care delivery and financial outcomes. Engaging employees in the improvement process fosters a sense of ownership and commitment, ultimately contributing to the organisation’s overall success and sustainability in the healthcare landscape. By prioritising continuous improvement, healthcare organisations can enhance their resilience and capacity to thrive in a competitive environment.
Frequently Asked Questions (FAQs) Regarding NHS Funding and Financial Growth
What are the primary sources of NHS funding?
The NHS is primarily funded through general taxation, national insurance contributions, and various government grants, which collectively support the provision of healthcare services throughout the UK. Understanding these funding sources is essential for comprehending the financial landscape of the NHS.
How do public-private partnerships benefit the NHS?
Public-private partnerships enhance the NHS by providing additional resources, facilitating infrastructure development, and introducing innovations that improve service delivery while reducing the financial burden on the public sector. These collaborations can lead to significant improvements in patient care and operational efficiency.
Why is long-term financial planning significant in healthcare?
Long-term financial planning is crucial for sustainability, enabling healthcare organisations to anticipate future demands, allocate resources effectively, and adapt to economic fluctuations in the healthcare environment. This proactive approach supports the overall health of the organisation and its ability to deliver quality care.
How can technology contribute to reducing healthcare costs?
Technology can streamline operations, improve patient care through telehealth services, and reduce administrative burdens, thus leading to significant cost savings for healthcare providers and organisations. By leveraging technological advancements, the NHS can enhance its efficiency and service delivery.
What role do grants play in supporting healthcare financial growth?
Grants provide essential funding for specific initiatives, allowing healthcare organisations to enhance services, invest in innovations, and improve overall financial performance and sustainability. By accessing these funds, organisations can bolster their capabilities and better serve their communities.
How important is staff training for financial growth in healthcare?
Training enhances workforce efficiency and service quality, leading to better patient outcomes, reduced turnover, and ultimately, improved financial health for healthcare organisations and systems. By investing in staff development, organisations can ensure they have the skills necessary to succeed in a competitive environment.
Can wellness programmes effectively attract more patients?
Yes, wellness programmes focus on preventive care, appealing to health-conscious individuals, and creating new revenue streams for healthcare providers through increased patient engagement and service utilisation. These initiatives foster a culture of health and well-being within the community.
Which KPIs are important for monitoring financial performance in healthcare?
Key performance indicators such as patient volume, average length of stay, and revenue per service line are vital for assessing financial health and operational effectiveness within healthcare organisations. By monitoring these metrics, organisations can make informed decisions to enhance their performance.
How can healthcare organisations secure investments from the private sector?
By presenting clear value propositions and demonstrating potential returns on investment, healthcare organisations can attract private sector investments to enhance their financial stability and growth prospects. This approach allows for mutual benefits and improved service delivery.
What continuous improvement strategies can be implemented in healthcare to drive success?
Strategies such as Lean and Six Sigma focus on process optimisation, enhancing efficiency, and fostering a culture of innovation to drive financial growth and sustainability in healthcare settings. By prioritising these methodologies, organisations can continuously improve their operations and patient care.
The post Healthcare Financial Growth Management: Successful Strategies appeared first on Healthcare Marketing Service.